Written by Thomas Greenfield
The global burden of low back pain (LBP) estimates, from the Global Burden of Disease 2010 study, [1], suggest that LBP causes more global disability than any other condition. With the ageing population, there is an urgent need for further research to better understand LBP across different settings.
Vos et al, UK 2015, suggests that over-50s are worst hit and that chronic back pain is made worse by our increasingly sedentary lifestyle, with the average Briton spending almost four hours a day on a phone or computer
THE STATISTICS:
4.2 million working days lost by workers aged 50-64 in 2014.
25-34 y/o 1.89 million days missed
35-49 y/o missed 3.86million days
Sick Days Due to Back Pain
7.7 million 2013
9.96 million 2015
11.8 million 2017
£1 BILLION lost in revenue every year in the UK due to lost sick days from low back pain.
The statistics are staggering!!
But what are the #solutions?
The medical approach simply has 3 options:
Do nothing and hope it goes away
Drugs – Orally or via Injections
Surgery
MEDICAL ROUTE:
| Opioids NSaids Nerve Blockers Muscle Relaxants Steriods |
|---|---|
2. Surgery | Fusion Removal |
Drugs essentially work in 2 ways:
BLOCK RECEPTORS (Non-competitive inhibition)
CHANGE ENZYME SHAPES (competitive inhibition)
THE MECHANISM OF ACTION OF SOME DRUGS ON THE MARKET IS ACTUALLY “UNKNOWN”. Eg: Paracetamol
The number 1 drug given over the counter for back pain is PARACETAMOL. The mechanism of action is not completely understood, but the main aim is to reduce pain or fever. Unfortunately, this comes with a whole host of adverse effects including liver damage, kidney damage, skin reactions, nausea, vomiting and reported causes of kidney cancer.
The cost of Paracetamol in the UK 2017 was:
Number of prescriptions | Total cost to NHS |
20,152,891 | £61,933,788.00 |
Looking at the Efficacy and safety of paracetamol for spinal pain and osteoarthritis: systematic review and meta-analysis of randomised placebo-controlled trials, in the British Medical Journal published In 2015, [2] it concluded that “Paracetamol is ineffective in the treatment of low back pain and provides minimal short term benefit for people with osteoarthritis”. It also concluded that “high quality evidence shows that patients taking paracetamol are 4 x more likely to have abnormal results on liver function tests compared with those taking oral placebo”. So, not only is it ineffective, it also causes abnormal liver tests. The research is clearly suggesting PARACETAMOL is not only useless in numbing low back pain, but also dangerous to your liver.

What about the number 1 drug prescribed by GPs for low back pain, OPIODS?
The aim of these drugs such as Tramadol, Zapain, or Codeine, is to create a feeling of numbness, or to dampen the pain.
Well, this comprehensive clinical review from the British Medical Journal in 2015 [3] stated that:
Opioids do not expedite return to work in injured workers or improve functional outcomes
For chronic back pain, systematic reviews find scant evidence of efficacy
The long-term effectiveness and safety of opioids are unknown
59% experienced adverse effects under 3 months
90% experienced adverse effects after 3 months
Adverse events reported were in the short term: constipation, nausea, sedation, and increased risk of falls and fractures. In the longer term: may include depression and sexual dysfunction, addiction (hyperalgesia), overdose related mortality and DEATH.
In Summary, there is NO evidence that reports you should take opioids for low back pain, the long-term effects on pain are unknown, but it will increase your chance of falls, fractures, depression, and overdose related death.
Doesn’t sound that appealing, does it?
What about anti-convulsant medications like GABAPENTIN?
Well, I am glad you asked. Since it affects the inhibitory neurotransmitter (GABA), it is effective at numbing every sensation in your nervous system, it is effectively a nerve blocker, but how it works is “unclear”. It has been successful in Side effect include fatigue, dizziness, headaches and wait for it…. SUICIDE!
Patorno et al (2010), [4] reviewed 297,600 people taking gabapentin: 801 attempted suicides >34.3 per 100 people reported suicidal thoughts
What about muscle relaxants?
Medically known as Benzodiazepines, the most common one is called DIAZEPAM ( AKA VALIUM). It enhances the effect of the neurotransmitter (GABA) resulting in sedative, hypnotic (sleep-inducing), anxiolytic (anti-anxiety), anticonvulsant , and muscle relaxant properties. Side effects include sleep problems, headaches and insomnia. One must be aware that if you take these drugs and you suddenly stop taking them, there is a very severe chance of DELIRUM TREMENS (AKA psychosis). These drugs are notoriously dangerous to come off due to the common induced psychosis one experiences when having withdrawal symptoms.
WHAT ABOUT STEROIDS?
There are 2 main types of steroids prescribed for low back pain Gluco-corticoids and mineral corticoids. They mimic the body’s natural hormones like cortisol to produce a reduction in inflammation. This slows the thyroid down. The most common prescribed steroid for pain is prednisolone. Side effects include weight gain, Gastro-intestinal ulcers, Headaches, sleep problems, and the big one…. osteoporosis.
Non-Steroidal Anti-inflammatories (NSAID’s)
Drugs like ibuprofen, Naproxen, Diclofenac work as either Cox 1 or Cox 2 inhibitors to close down the receptor sites that modulate the inflammation within the body. These drugs are non-specific, which means they cannot target a particular place like low back pain. They affect every receptor in the body that is responsible for inflammation.
The most commonly prescribed NSAID for low back pain is Ibuprofen [5]. However, the NICE guidelines clearly state that they must only be used in the short term (less than 2 weeks) to aid return to activity. Long term use is absolutely NOT recommended, and is associated with Cardiovascular risks, Gastro-intestinal problems & joint degeneration, and causes adverse CNS effects compared to placebos.
DRUGS FOR LOW BACK PAIN IN SUMMARY:
Looking at all the drugs, there was a comprehensive systematic review in 2022 [5], where they looked at what drugs were being prescribed based on whatever was the GP’s preferred opinion was for low back pain patients.
They concluded that there was disagreement in interpreting the literature, and nobody can agree on what to prescribe, except that ibuprofen is normally recommended first. This is somewhat hilarious considering the NICE Guidelines, because as we have just read, there is no research to support ibuprofen for chronic low back pain.
Whilst we mention the NICE guidelines, let me explain what they are. NICE guidelines are evidence-based recommendations for health and care in the UK. They set out the care and services suitable for most people with a specific condition or need, and people in particular circumstances or settings. These guidelines are there to help health and social care professionals to: prevent ill health.
So why are we not following the guidelines for chronic low back pain?
INJECTIONS FOR LOW BACK PAIN?
Again, the NICE GUIDELINES clearly advise
Do not offer spinal injections for managing chronic low back pain.
Consider epidural injections of local anaesthetic and steroid in people with acute and severe low back pain
They do provide a small, short-term reduction in pain, however there is no difference between placebo and spinal injections. On a positive note, and unlike the harmful drugs we outlined earlier, the injections have no serious side effects; they are just a waste of our precious NHS money.

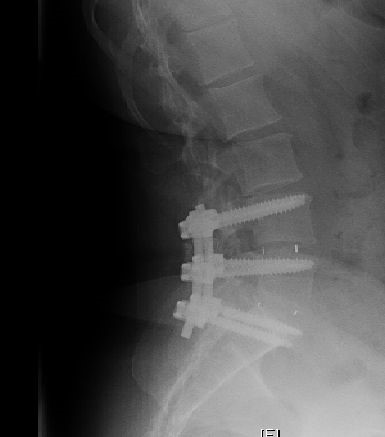
WHAT ABOUT FUSION SURGERY FOR CHRONIC LOW BACK PAIN?
A Cochrane review of surgical fusions for back pain in 2016 concluded there are no published randomised controlled trials which established effectiveness of fusions for chronic pain.[6]
Most of the research was criticised for measuring short term pain; not long-term outcomes: there is no research of long-term outcomes of spinal fusion. The incidence of persistent post-operative pain syndrome was as high as 40% and that there was a 50% success rate, at best, from the first operation, 30% from the second and 15% from the third.
There was one Four-year follow-up of surgical versus non-surgical therapy for chronic low back pain by Jens Ivar et al (2009), who concluded that long-term improvement was not better after fusion compared with cognitive intervention and exercises. [7]
WHAT ABOUT DECOMPRESSION SURGERY?
Also known as laminectomies or discectomies, these surgeries do have better evidence that fusion (unsurprisingly). The most recent systematic review found at 2 years 66% of people showed lower pain & disability [8].
5-year study shows lower pain, but social function was worse.
No trials were identified comparing surgery to no treatment or placebo/sham. This means that surgery has NEVER been compared to fake surgery. WHY NOT? Perhaps the small amount of success seen from surgery is actually due to the placebo effect of the significance of the surgery itself.
IN SUMMARY, SURGERY OR NOT?
THE most recent review [9] published in 2021 in the Lancet (a well-respected medical journal), stated we cannot conclude on the basis of current evidence whether surgical or non-surgical treatment is better for individuals with lumbar spinal stenosis.
So exactly what should you be doing for your chronic low back pain?
Without question, and undeniably within the research, the most effective, safest, and most cost effective with the best long-term outcomes is manual therapy and exercise.
The most recent comprehensive review in 2021 [10] concluded there was good evidence for Acupuncture, Tai Chi, and spinal manipulation for low back pain.
Particularly and the reason why we provide Chiropractic, the research supporting chiropractic for chronic low back pain is outstanding. Way back in 1993, Manga, et al. (1993). Provided The Manga Report, an Independent Report Commissioned by the Ontario Provincial Government, into the effectiveness and cost-effectiveness of chiropractic management of low-back pain.
It concluded:
“There is an overwhelming body of evidence indicating that chiropractic management of low- back pain is more cost-effective than medical management. We reviewed numerous studies that range from very persuasive to convincing in support of this conclusion. The lack of any convincing argument or evidence to the contrary must be noted and is significant to us in forming our conclusions and recommendations.”
The cost advantages for chiropractic for matched conditions appear to be so dramatic that Manga, in his second report, concluded that doubling the utilization of chiropractic services from 10% to 20% may realize savings as much as $770 million in direct costs and $3.8 billion in indirect costs.
IN terms of ongoing chiropractic, one study [11], concluded that intensive spinal manipulation is effective for the treatment of chronic low back pain. This experiment suggests that maintenance spinal manipulations after intensive manipulative care may be beneficial to patients to maintain subjective post intensive treatment disability levels. Future studies, however, are needed to confirm the finding in a larger group of patients with chronic low-back pain.
Another study, [12], showed that SMT is effective for the treatment of chronic nonspecific LBP. To obtain long-term benefit, this study suggests maintenance SM after the initial intensive manipulative therapy.
So, in summary, regular long term spinal manipulation is effective at managing long term low back pain. It’s the safest, most cost effective and the best long-term outcomes if you receive it regularly. Some people will say it is something that you “have to have forever”, but if that is having positive effects on your health, why is that a bad thing? You wouldn’t say that about exercising because you “have to go forever on a weekly basis for it to have an effect”.
I hope this comprehensive, balanced blog provides you with a better understanding of the medical business machine and the easy things you can do to manage your low back pain.
(PDF) The global burden of low back pain: Available from: https://www.researchgate.net/publication/261070129_The_global_burden_of_low_back_pain_Estimates_from_the_Global_Burden_of_Disease_2010_study [accessed Jul 27 2018].
Efficacy and safety of paracetamol for spinal pain and osteoarthritis: systematic review and meta-analysis of randomised placebo controlled trials, in the British Medical Journal published In 2015, BMJ 2015; 350 doi: https://doi.org/10.1136/bmj.h1225 (Published 31 March 2015)Cite this as: BMJ 2015;350:h1225
Opioids for low back pain, BMJ 2015; 350 : https://doi.org/10.1136/bmj.g6380 (Published 05 Jan 2015)
Patorno et al (2010): Anticonvulsant Medications and the Risk of Suicide, Attempted Suicide, or Violent Death; JAMA. 2010;303(14):1401-1409. doi:10.1001/jama.2010.410
Price, M.R., Cupler, Z., Hawk, C. et al. Systematic review of guideline-recommended medications prescribed for treatment of low back pain. Chiropr Man Therap 30, 26 (2022). https://doi.org/10.1186/s12998-022-00435-3
Surgical management of low back pain Leigh Atkinson and Andrew Zacest Med J Aust 2016; 204 (8): 299-300. || doi: 10.5694/mja16.00038 Published online: 2 May 2016
Eur Spine J. 2007 Nov; 16(11): 1842–1847. Published online 2007 May: The outcome of spinal decompression surgery 5 years on
Effectiveness of Surgery for Lumbar Spinal Stenosis: A Systematic Review and Meta-Analysis. Gustavo C. Machado ,et al, Published: March 30, 2015 https://doi.org/10.1371/journal.pone.0122800
Xing Du, Yunsheng Ou et al, (2001), The evidence gap in low back pain management strategies, The Lancet, VOLUME 398, ISSUE 10306, P1131, SEPTEMBER 25, 2021, https://doi.org/10.1016/S0140-6736(21)01821-3
Urits, I., Schwartz, R.H., Orhurhu, V. et al. A Comprehensive Review of Alternative Therapies for the Management of Chronic Pain Patients: Acupuncture, Tai Chi, Osteopathic Manipulative Medicine, and Chiropractic Care. Adv Ther 38, 76–89 (2021). https://doi.org/10.1007/s12325-020-01554-0
Efficacy of preventive spinal manipulation for chronic low-back pain and related disabilities: a preliminary study. Descarreaux M, et al. J Manipulative Physiol Ther. 2004.




Comments